Introduction
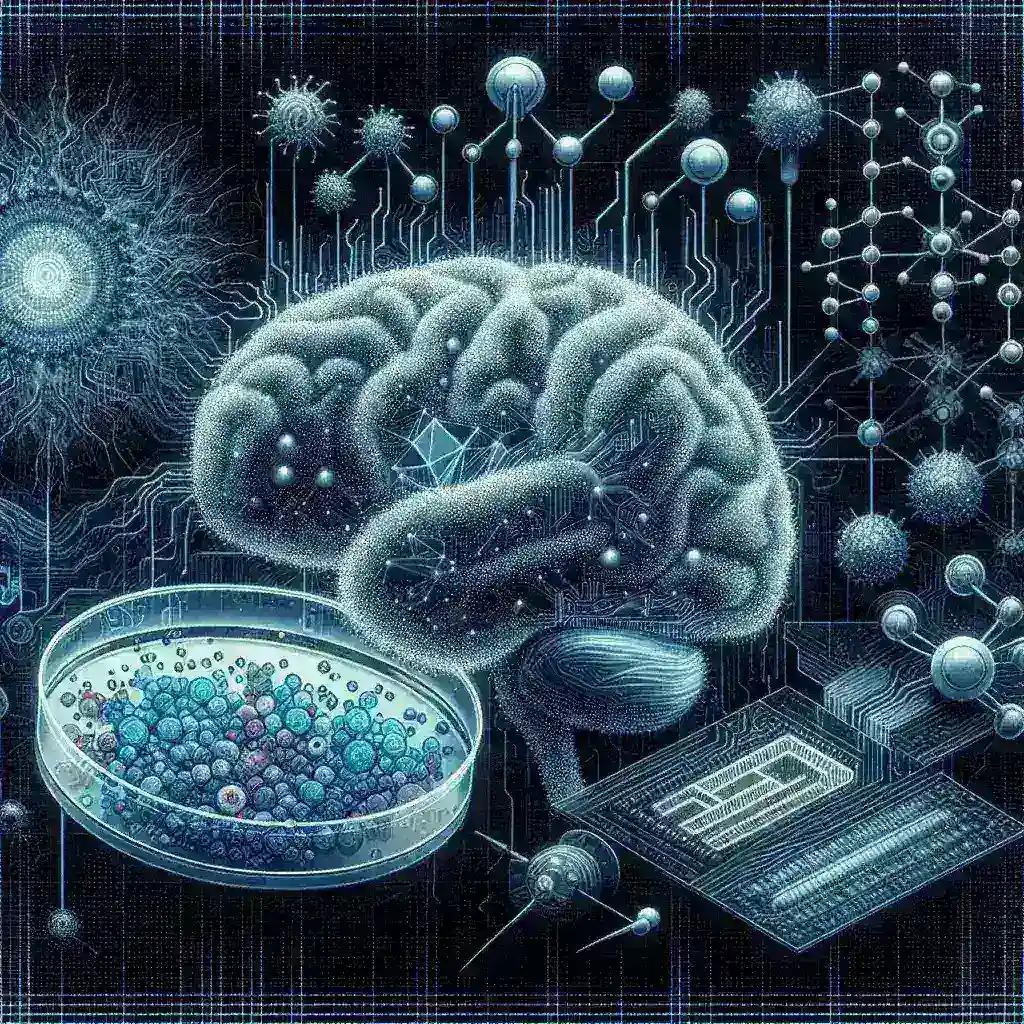
In recent years, the intersection of artificial intelligence (AI) and neuroscience has paved the way for groundbreaking advancements in psychiatric drug testing. One of the most promising developments in this area is the use of AI-powered brain organoid models. These miniature brain-like structures, derived from human stem cells, mimic the complexity of the human brain, offering researchers an unprecedented platform for studying psychiatric disorders and testing potential drug therapies.
The Genesis of Brain Organoids
Brain organoids, often referred to as “mini-brains,” were first developed in the early 2010s. These organoids are three-dimensional cultures that replicate specific aspects of brain architecture and function. Created from pluripotent stem cells, they can differentiate into various types of neural cells, providing a versatile model for studying neurodevelopmental and neurodegenerative diseases.
Development and Advancements
- Initial Breakthroughs: The first successful organoids were generated by researchers at the University of Cambridge. By 2013, they had created cerebral organoids that provided insights into brain development and congenital brain disorders.
- Integration of AI: The integration of AI into this research has accelerated the understanding of brain organoids. AI algorithms can analyze vast amounts of data generated from these models, identifying patterns and predicting outcomes more efficiently than traditional methods.
- Ethical Considerations: While these advancements are promising, they also raise ethical questions about the use of human-derived models. Researchers are striving to balance scientific progress with ethical responsibilities.
AI’s Role in Enhancing Drug Testing
AI plays a crucial role in enhancing the efficacy and accuracy of drug testing using brain organoids. By utilizing machine learning algorithms, researchers can:
Predict Drug Responses
AI systems can analyze the genetic and molecular profiles of organoids to predict how they will respond to various psychiatric drugs. This predictive capability streamlines the drug discovery process, allowing for faster identification of viable candidates for clinical trials.
Optimize Drug Formulations
Using AI, researchers can simulate various drug formulations and dosages to determine the most effective treatment strategies. This optimization process reduces the likelihood of trial and error in clinical settings, ultimately saving time and resources.
Personalized Medicine
AI-powered organoids facilitate the development of personalized medicine approaches. By creating organoids from individual patients’ cells, researchers can tailor drug therapies to meet specific genetic and biological profiles, enhancing treatment outcomes.
Challenges and Limitations
While the potential of AI-powered brain organoid models is immense, there are several challenges that researchers must navigate:
Complexity of Psychiatric Disorders
Psychoactive drugs often target intricate neural pathways, and replicating this complexity in organoids is a significant challenge. Current models may not fully capture the nuanced interactions of neural circuits involved in psychiatric conditions.
Scalability of Organoid Production
Producing brain organoids at scale for widespread testing is another hurdle. Researchers are exploring automation and bioreactor technologies to increase the efficiency of organoid production.
Data Interpretation
As AI systems analyze vast datasets, the interpretation of results can be complex. Ensuring that findings are accurate and clinically relevant requires ongoing validation and refinement of algorithms.
Future Directions
The future of psychiatric drug testing using AI-powered brain organoid models is bright. Researchers are optimistic about several developments:
Enhanced Models
Future advancements in organoid technology will likely lead to even more complex and representative models of the human brain, allowing for better understanding of psychiatric conditions.
Integration with Other Technologies
Combining organoid models with other technologies, such as CRISPR gene editing and optogenetics, could further enhance the study of psychiatric disorders.
Global Collaborative Efforts
International collaborations between research institutions, universities, and pharmaceutical companies will accelerate the development of these technologies, promoting a more integrated approach to mental health research.
Conclusion
AI-powered brain organoid models are revolutionizing the landscape of psychiatric drug testing, offering innovative approaches to understanding and treating mental health disorders. While challenges remain, the potential for personalized medicine and improved drug efficacy is paving the way for a brighter future in psychiatric care. As we continue to explore this intersection of technology and neuroscience, the possibilities are as vast and intricate as the human brain itself.